Corneal Implants
IOB translational project
Corneal dystrophies are inherited degenerative eye conditions, and a major cause of blindness. Abnormal cellular function and development leads to excess fluid in the cornea, the central transparent front-most part of our eyes, covering the iris and pupil.
Fuchs’ [[‘fooks’]] endothelial dystrophy is affecting the innermost layer of the cornea, with fluid starting to seep into the cornea leading to distorted vision. It affects up to 4% of people aged over 40, women more often than men. It was first discovered by an Austrian ophthalmologist named Ernst Fuchs in 1910.
Corneal transplantation is the current standard of care: in a partial thickness cornea transplantation the host Descemet membrane and endothelium are replaced by donor Descemet membrane and endothelium.
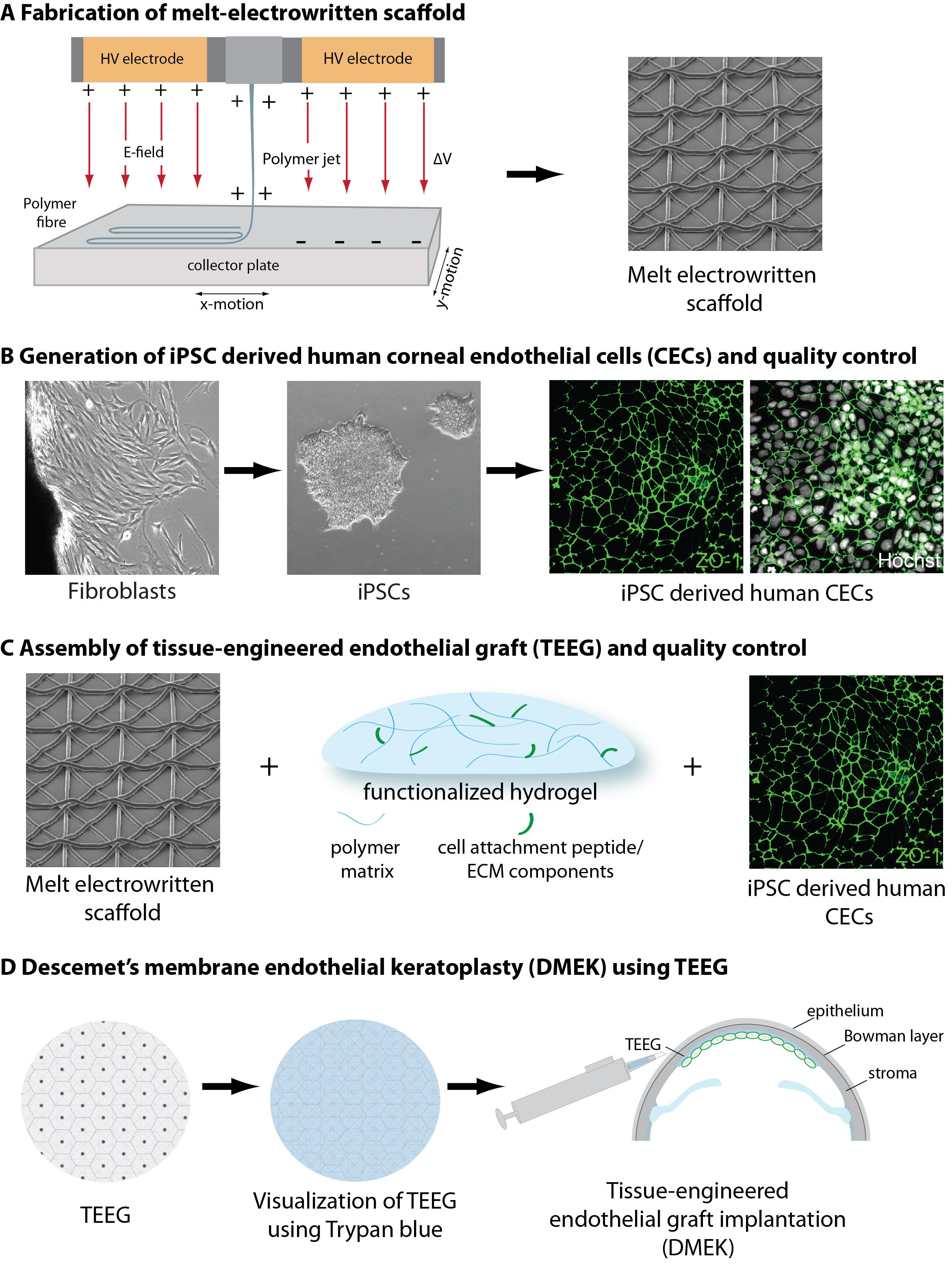
As not enough donors are available to treat all patients in need, IOB, in collaboration with the lab of Pierre Balmer from the Department of Biomedicine (DBM) of the University of Basel, and Zisis Gkatzioufas, senior physician at the Basel University Eye Clinic leading the division of cornea and refractive surgery, plans to combine biofabrication (3D printing) with stem cell technology, to generate a bioimplant as drop-in replacement for transplantion of Descemet’s membrane.
The interdisciplinary team is producing scaffolds to establish human corneal endothelial cells from inducible pluripotent stem cells (iPSCs), and is trying to combine cells and scaffolds.
Team Members Corneal Implants Project
| Pierre Balmer | Project lead lab science (DBM, UniBas) |
| Zisis Gkatzioufas | Project lead clinical science (USB, Eye Clinic) |
| Lisa-Marie Anders | Postdoc |
| Magdalena Renner | Head Organoid Platform IOB |